WHAT IS A PORT A CATH
Port-A-Cath is an implanted venous access device, also known as an implanted port, placed completely under the skin. It is used for patients who require frequent or continuous chemotherapy administration.
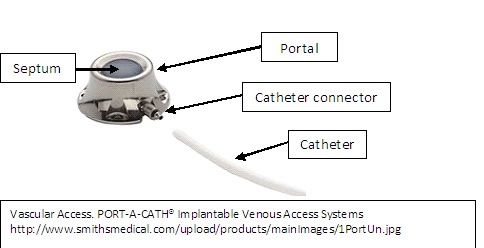
The Port consists of three parts:
-The portal: a small chamber sealed with a septum on the top, made of silicone
-The catheter: a thin flexible tube
-The catheter connector: connects the catheter to the portal
Why is a Port-A-Cath used in chemotherapy?
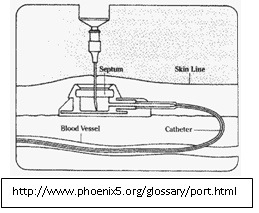
The catheter of the port sits inside a large central vein. The port is used to collect blood samples and to give chemo medications. Before using, the skin over the port is cleaned and then a special needle is used to puncture the septum of the port, which is connected to the catheter. This allows for collection of blood samples as well as direct administration of medication into the bloodstream, using the port. After every infusion/injection, the port is flushed with heparin solution or once every 4 weeks if the port is not used regularly.
How is the Port-A-Cath used?
Generally chemotherapy drugs are very toxic and irritating to the skin, tissues and veins. Giving such potent medications into a small vein can irritate and cause inflammation of these blood vessels, resulting in long-term scarring and blockage of these veins. Also, giving chemo into a small vein allows the medication to leak into the nearby tissues and cause tissue damage. As a result, such medications are administered into a large central vein so that they can be immediately diluted by a large volume of blood and be delivered effectively throughout the entire body. The chemotherapy drugs are usually administered into the Internal Juglar or Subclavian vein; but sometimes Brachial vein may also be used. Studies show that the use of the Port-A-Cath in treatment & management of cancer patients, results in shorter hospital stay, less nursing time spent trying to access veins, preservation of the small veins, fewer emergency visits, decreased cost of therapy and overall greater patient satisfaction. As a result, the port serves a safe and effective route of giving chemotherapy drugs.
How is the Port placed?
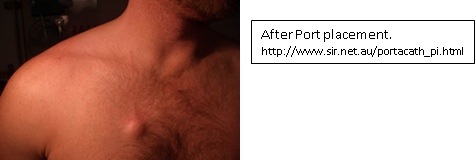
Placing the Port is a small surgical procedure and takes less than an hour. It is performed by surgeon in theatre. The procedure involves a 3cm skin incision on the chest wall for the port pocket and 5mm incision in lower neck to enter the vein. The port is placed completely inside the body. One end of the catheter is inserted into the vein while the other end is connected to the portal, under the skin. The tip of the catheter lies in a vein just above the heart.
Port placement:
Chest-placed system: The Port is placed in the chest and the catheter is inserted into a vein in the chest. The tip of the catheter lies in a vein just above the
Generally, the patients can go home two hours after the procedure or after the effect of sedation has worn off. However, patients are advised to not drive or operate any machinery for 24 hours. When the incisions are healed, one can notice a small bump under the skin.
What preparations are required for the port implantation?
One is asked to not eat or drink anything starting at midnight before the procedure day. Clear fluids and medications are allowed till the time of procedure but it is best to verify with your doctor. Also mention to your doctor if you are on aspirin, plavix or warfarin to find out when to discontinue these medications prior to surgery. The medications can be resumed the day after the procedure. If you are sick with an active/ongoing infection, your doctor might choose to postpone your Port placement.
What are the aftercare precautions required?
-Keeping the port-site clean at all times is very crucial. If an access needle is in place, it is covered with a dressing to keep the site clean and prevents the needle from dislocating. If there is no needle in place, one can bathe/shower regularly.
-After surgery, it is normal to have some redness and tenderness at the area of incision which should resolve in 24-48hrs. However if you continue to have redness, tenderness, swelling or drainage from the site for more than 2-3 days or notice any other unusual skin changes, contact your doctor immediately.
-Avoid any strenuous activities involving the chest/arms for at least ten days. If the port is not used in 7 days after placement, follow-up with your doctor for a wound check and dressing change.
-If your portacath is no longer being used, you need to follow-up with your doctor every 4 weeks and get it flushed with saline water and locked with heparinized saline to prevent formation of blood clots.
-Minimize physical activities that involve excessive, repetitive upper extremity motion: such as swimming, golfing, weight-lifting as there is risk of catheter damage/ fragmentation (breaking). Check with your doctor to make sure you take proper precautions while engaging in such activities.
What are the potential problems /risks associated with Port-A-Cath?
-Risk of infection: although the risk of infection with the port is minimal, catheter-related bloodstream infection is a concern in cancer patients. This can be prevented by keeping the port site clean, using antimicrobial catheters and antibacterial solutions to flush the catheter. If infected, the port is removed and one is treated with appropriate antibiotic medications.
-Risk of forming clots: After months of insertion, clots can form in the catheter. This is prevented by flushing the catheter regularly after blood draws and not giving any contrast through the port. Patients do not need to be on any treatment to prevent clot formation in the Port-A-Cath.
-Air outside the lungs: at the time of port placement air can leak out of the lungs but usually resolves with time.
-Irritation or blistering of skin where chemotherapy is being given
-Catheter dislocation if not properly secured with sterile tapes or surgical strips
-With the use of modern imaging technology, there is very little risk of bruising, bleeding or damage to the blood vessels.
How long does the Port-A-Cath need to stay in place?
The port can stay as long as your doctor wants. Talk to your doctor or nurse about how long your port needs to stay in place.
Is it ok to have MRI with the Port in place?
Port-a-cath is MRI conditional, which means that they may safely undergo magnetic resonance imaging with magnetic field strength of 3.0 or lower. However do mention that you have a port-a-cath placed prior to having an MRI done.
Will it be ok to go through security alarms/metal detectors with a port?
Metal detectors will not harm the Port-A-Cath. The Port will not activate the security alarms. However since the sensitivity of metal detectors varies, it might be helpful to have your Port Identification Card with you.
Additional guidelines for your Port.
-Do not inject any fluids or solutions in your port unless you have been asked to do so by your doctor or nurse.
-Inform your doctor if you notice that fluids are not flowing freely through the port and stop any infusion at that time.
-Inform your doctor if you notice any skin changes, such as redness, swelling, or drainage at the site of Port placement.